Understanding Sperm Donation: How the Process Works, Who Can Donate, and What to Expect
Sperm donation plays a crucial role in helping individuals and couples achieve their dreams of parenthood when natural conception isn't possible. This medical process involves healthy men providing genetic material to assist others in building families through assisted reproductive technologies. The donation process requires careful screening, medical evaluations, and ongoing commitment from donors who meet specific health and lifestyle criteria. Sperm donation has become an increasingly important component of reproductive medicine, offering hope to countless individuals and couples facing fertility challenges. The process involves rigorous medical and psychological screening to ensure the safety and viability of donated genetic material for use in assisted reproductive procedures.
Sperm donation has become an increasingly important option for individuals and couples facing fertility challenges, single parents, and same-sex couples seeking to build families. The process involves careful medical screening, legal considerations, and ethical guidelines designed to protect all parties involved. For those considering donation, understanding the requirements, procedures, and implications is essential.
Understanding Who Can Become a Sperm Donor
Becoming a sperm donor requires meeting specific health, age, and lifestyle criteria established by fertility clinics and sperm banks. Most facilities accept donors between the ages of 18 and 39, though some extend this range to 45. Candidates must be in good physical and mental health, free from genetic disorders, and maintain a healthy lifestyle without substance abuse. Educational background, height, and family medical history are often considered during the selection process. The acceptance rate for sperm donors is relatively low, with many clinics approving only 1-5% of applicants due to stringent quality standards. Donors typically undergo preliminary questionnaires assessing their medical history, lifestyle habits, and motivation before advancing to more detailed evaluations.
Why People Choose to Donate Sperm
Motivations for sperm donation vary widely among individuals. Many donors are driven by altruistic desires to help others experience parenthood, particularly those who have witnessed friends or family members struggle with infertility. Financial compensation also serves as an incentive, though it should not be the sole motivator according to ethical guidelines. Some donors appreciate the opportunity to undergo comprehensive health screenings at no personal cost, gaining valuable insights into their own fertility and genetic health. Others find meaning in knowing their contribution can create families and bring joy to people who might otherwise be unable to conceive. The decision often reflects a combination of these factors, with donors feeling a sense of purpose in supporting reproductive choices for diverse family structures.
The Medical Screening and Evaluation Process
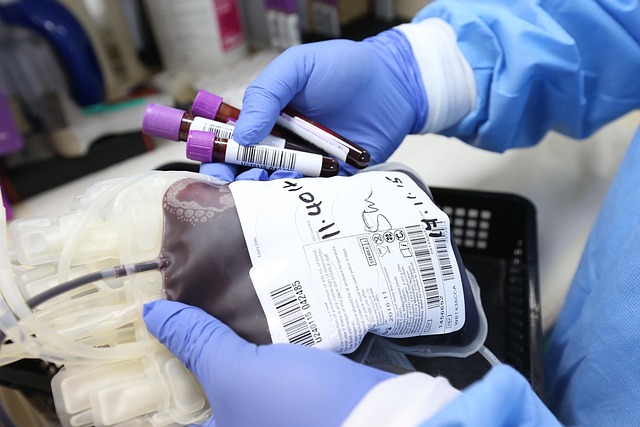
The screening process for sperm donors is thorough and multi-staged, designed to ensure the highest quality samples and minimize health risks. Initial screening includes detailed questionnaires about personal and family medical history, genetic conditions, and lifestyle factors. Physical examinations assess overall health, while blood and urine tests screen for infectious diseases including HIV, hepatitis B and C, syphilis, and other sexually transmitted infections. Genetic testing identifies carriers of hereditary conditions such as cystic fibrosis, sickle cell anemia, and Tay-Sachs disease. Semen analysis evaluates sperm count, motility, morphology, and post-thaw viability, as samples must withstand the freezing and thawing process. Psychological evaluations ensure donors understand the implications of their decision and are emotionally prepared for the process. This comprehensive screening typically takes several weeks to months, with ongoing testing required throughout the donation period to maintain safety standards.
Privacy and Confidentiality in Sperm Donation
Privacy protections in sperm donation vary significantly depending on jurisdiction and the type of donation arrangement chosen. Anonymous donation historically represented the standard approach, where neither donor nor recipient families know each other’s identities. However, many regions now offer identity-release or open donation options, where donor-conceived children can access identifying information upon reaching adulthood, typically at age 18. Some arrangements involve known donors, where the donor and recipient family have pre-existing relationships or meet through the process. Clinics and sperm banks maintain strict confidentiality protocols regarding donor information, though legal frameworks differ internationally. Donors should carefully consider their comfort level with potential future contact and understand that DNA testing services have made complete anonymity increasingly difficult to guarantee. Contracts typically outline privacy expectations, rights, and limitations, though legal precedents continue to evolve as technology and social attitudes change.
Legal and Ethical Considerations
The legal landscape surrounding sperm donation involves complex considerations that vary by country and region. In most jurisdictions, donors who contribute through licensed clinics or sperm banks have no legal parental rights or financial responsibilities toward resulting children. However, private arrangements outside medical facilities may not offer the same legal protections, potentially exposing donors to paternity claims and child support obligations. Contracts between donors, recipients, and fertility clinics establish clear expectations regarding anonymity, future contact, and parental rights. Ethical guidelines emphasize informed consent, ensuring donors understand the potential outcomes of their contribution, including the possibility of multiple offspring. Some countries limit the number of families that can use sperm from a single donor to reduce the risk of accidental consanguinity among donor-conceived individuals. Donors should seek legal counsel to understand their rights and obligations fully, particularly regarding evolving laws around donor anonymity and the rights of donor-conceived individuals to access genetic information.
Sperm donation represents a meaningful way to help others build families while contributing to reproductive medicine. The process requires commitment, patience, and careful consideration of medical, legal, and ethical dimensions. Potential donors should research facilities thoroughly, understand all requirements and implications, and ensure their motivations align with the responsibilities involved. By meeting rigorous standards and following established protocols, donors play a crucial role in making parenthood possible for many individuals and couples worldwide.